Connect With Us
Blogs

Health Tips (46)
February is American Heart Month, and at Superior Foot & Ankle Care Center, we want to recognize this important opportunity for our Douglas Park/Los Angeles County area patients to make healthy changes to reduce the risk of heart disease. Did you know that symptoms of heart disease may show themselves in your feet? Swelling in the lower legs, feet, and ankles and a bluish or purplish discoloration of the skin on your feet and toes may be indicators of a heart problem. If you notice any of these symptoms, it’s important that you contact our Long Beach office for an appointment so that our podiatrists, Dr. Victoria M. Foley and Dr. Constance Ornelas, can examine your feet and determine the cause of these changes in your feet.
Show Your Love
With hearts abounding for Valentine’s Day, we’d like to suggest some heart-healthy ways to celebrate with the ones you love. After all, spending time together in good health is the best gift of all.
Here are a few ideas:
- Take a Dance Class—Romance is in the air when you and your beloved take to the dance floor. And you’ll also be getting exercise. Staying active is a key factor in reducing the risk of heart problems.
- Cook a Delicious Dinner Together—Healthy eating doesn’t have to be boring! Fill your plates with a colorful array of vegetables and fruits. Incorporate lean proteins like skinless chicken and fish into your menu. Experiment with cuisines from around the world. Add flavor instead of fat with exotic seasonings. Light the candles, and you’re all set!
- De-Stress Times Two—Stress increases blood pressure and puts extra strain on your heart. Find new ways to relax together. Splurge on a couple’s massage. Take a long walk in a new park or part of the city you haven’t been to before. Pray or meditate together.
Cultivating healthy habits with the one you love will help ensure a long life together. For more ways to be proactive about your podiatric health, contact us by calling: (562) 420-9800.
At Superior Foot & Ankle Care Center, we support a whole-body approach to foot health. February is American Heart Month. Part of keeping your heart healthy is eating correctly to maintain a healthy weight and staying active. Your feet play a key role in an active lifestyle. But, if the rest of your body isn’t being properly cared for, your feet can’t do it on their own. Below are areas that need your attention to in order to have good heart, foot, and overall body health.
Stress Busting—negative stress not managed correctly can lead to a lack of motivation and caring about our health. It’s easy to throw aside your exercise program because you’re in a bad mood or sad. Cultivate tools that can help you reduce stress and get you back on track:
- Practice positive self-talk. If you stop and listen, we’re talking to ourselves all the time in our heads. When stressful things occur, you can start to change your outlook by changing your self-talk. Instead of “I can’t believe this is happening,” try “Okay, I can handle this. The first step is…” or “There’s no way I can do this,” change to “Where can I find help with this issue?”
- When stressful situations hit, put some space between yourself and the situation. Take a walk, spend some time with a pet or even count to 10 and do some deep breathing exercises to help you get under control.
- Cultivate ongoing stress-reducing activities such as hobbies, prayer, getting together with friends, reading, home improvement or gardening project.
Sleep it Off—not getting enough sleep (and enough is defined as 7-9 hours a night) can negatively impact your mood, eating habits, mental sharpness, physical functioning and more. Try some of these tips for a better night’s sleep:
- Set your cell phone on silent or do not disturb and don’t keep it close to your bed. Falling asleep to your Facebook feed is not restful.
- If you like to fall asleep while watching television, make sure you set it on a timer to go off. Studies show that sleep is less deep when a flashing screen plays all night in your room.
- Take time to wind down before bed. A cup of decaffeinated tea, warm shower or bath, and some light reading are all excellent ways to relax and prepare for sleep. Establishing a routine before bed helps signal your body it’s sleep time.
Your feet work in conjunction with your heart and the rest of your body to achieve good health. If you have concerns about your feet, make an appointment to see one of our podiatrists, Dr. Victoria Foley or Dr. Constance Ornelas, at our Long Beach office by calling: (562) 420-9800.
February is American Heart Month and we at Superior Foot & Ankle Care Center want to encourage an activity that will benefit your heart as well as your feet: walking. According to the American Heart Association, brisk walking can lower your risk of diabetes, high blood pressure, and high cholesterol—three factors that greatly increase your risk of heart disease. All of these types of disorders can negatively impact your circulation. With your feet being the part of your body farthest from your heart, circulatory issues are particularly important to good podiatric health. In addition, walking helps you maintain a healthy weight—another plus for protecting your heart and your feet. So, what are you waiting for? Below are a few tips to help you get started.
- Start with good shoes. Walking is appealing because it doesn’t require a lot of expensive equipment and you can do it practically anywhere. The one thing you do need, however, is a good pair of shoes. It’s best to get your feet professionally measured at a shoe store that specializes in athletic footwear. If you have an existing foot disorder such as bunions or plantar fasciitis, talk to one of our podiatrists, Dr. Victoria Foley or Dr. Constance Omelas to learn about designs that will best accommodate your condition. The foot doctor may prescribe an orthotic device to improve comfort and function of your feet.
- Pace yourself. While 30 minutes a day is the goal, every step puts you on the path to better health. If you’ve been sedentary for a while it’s a good idea to start small and gradually increase the speed and length of your walks. Can’t find 30 consecutive minutes? Take two 15-minute walks. Look for ways to sneak in extra steps: walk while you talk on the phone, park farther away from the office or stores, take the stairs instead of the elevator or escalator.
- Make it enjoyable. Walk and talk with a friend, watch your favorite television series while on the treadmill or make walking a bonding opportunity with your teenager. You are much more likely to stick with an activity if you like it.
Within a short time, your walking program will begin to pay off. Not only will your heart and feet be healthier, you’ll sleep better and be more focused during the workday. If you have additional questions about walking and your feet, contact our Long Beach office by calling: 562-420-9800.
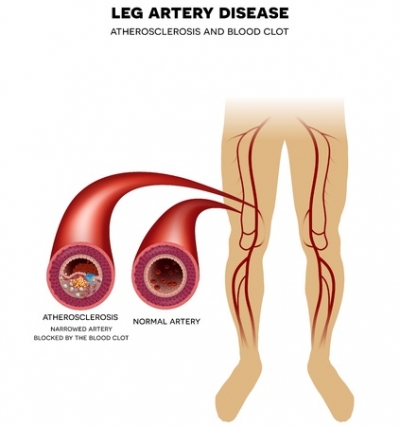
February is National Heart Month and here at Superior Foot & Ankle Center we want patients to understand the vital connection between heart and podiatric health. High blood pressure, or hypertension, is a major contributing factor to heart disease. Hypertension can lead to peripheral artery disease and other circulation problems which can have a significant impact on your feet. Poor circulation, particularly in patients with diabetes can lead to sores and ulcers forming on your feet and increase the risk of amputation. Here are some other facts about hypertension:
- 90 percent of American adults are expected to develop high blood pressure during their lifetimes
- It’s the number one risk factor in women’s deaths in the U.S. and the number two for men
- High blood pressure is more prevalent in blacks than whites and also develops earlier in life
Fight Back
There are a number of ways that you can help reduce your risk of hypertension:
- Know your numbers—get your blood pressure checked regularly
- Maintain a healthy weight—add more colorful fruits and vegetables to your plate, reduce carbs and sugars
- Exercise regularly—look for small ways to increase activity: park farther away from your office entrance, pace while you talk on the phone
- Reduce sodium in your diet—read labels and make more meals at home using herbs, non-sodium seasonings, citrus fruits and other flavorful ingredients to spice up your dishes
- Limit alcohol intake
- Don’t smoke
- If your doctor prescribes medication for hypertension take as directed
If you have not been diagnosed with hypertension but you are experiencing cramping in your feet or changes in feet’s skin color or temperature, make an appointment at our Long Beach office by calling: to see one of our podiatrists, Dr. Victoria M. Foley or Dr. Constance Ornelas. These may be early warning signs of high blood pressure or another condition that the foot doctor will want to evaluate.
Do you ever have those mornings when you’re in a rush, so you don’t have all the time you need to properly perform your skin care regimen? On one of those mornings have you ever secretly used your hand or foot skin cream on your face?
You probably think “What’s the harm?” Here’s a look at why all skin creams aren’t the same and what you should be using to treat dry feet.
Skin Cream: Is Each One Equal When It Comes to Your Feet?
The simple answer is no, not all skin creams are created equal because each skin cream is designed to treat specific areas of the body. By their nature, the skin of your face and that of your hands or feet aren’t the same. The skin on your face is more delicate, while the skin on your hands and feet is thicker. Skin is actually different everywhere, which means different care and different formulas.
Hand and foot creams may have the same basis as face creams, and they have ingredients in common, but they have different concentrations of them, which is what makes all the difference.
Hand and foot creams need to work as barriers. For this, they need to have high concentrations of wax, greases, oils, and chemical exfoliating agents. If you use them on your face, you risk causing blocked pores and pimples. So, while you can use a face skin cream on your feet or your hands, you shouldn’t do it the other way around—even if you have a tiny dry patch. Foot and hand creams are just too rich, thick, and sticky to be applied to your facial skin.
Treating Dry, Cracked Feet at Home
With the cold weather just over the horizon, so too are dry feet. Here are some tips on how you can treat dry, cracked feet at home:
- Wash feet daily with warm, soapy water. Don’t use hot water because it dries out skin. Hot water is also harmful to diabetics and anyone else with impaired circulation to the feet.
- Exfoliate the feet, especially the heels, while washing. Use a warm cloth or pumice stone, and rub the skin gently to slough off dead skin.
- Dry feet thoroughly. Dry well between the toes since fungus and bacteria like to grow in warm, moist, dark places.
- Moisturize daily. Try using products containing urea, which is naturally present in skin cells. Using a product that has urea increases the skin’s ability to hold in moisture. Avoid moisturizer between the toes. Put on cotton socks after moisturizing.
- Soak your feet. Limit foot soaks to 10-15 minutes, three times a week. Soaking for long periods of time can dry out your feet. Use a solution of ¼ cup white vinegar and enough warm water to cover the feet up to the ankles. The mild acetic acid in vinegar softens skin.
Making Your Own Moisturizer
Here are some easy home-made moisturizers that can help heal dry, cracked feet.
Coconut Shea Butter—combine ¾ cup coconut oil with ½ cup shea butter in a sauce pan and place on low heat. Once they’ve melted, remove from the heat and stir in 15 drops of lavender essential oil. Store in a glass jar with a lid somewhere cool. Massage this foot moisturizer into feet, focusing on dry, cracked areas. Cover feet with cotton socks right away. Try this once in a while for some nice pampering or repeat on a regular basis to soften dry feet.
Honey Foot Cream—warm 1 cup of organic honey slightly to make it easier to spread. Stir in 2 tablespoons of warm milk and the juice of ½ an orange. Use a pumice stone or foot file to slough off some of the callused skin before spreading a layer of mixture evenly onto your heels, massaging as you go to help it sink in. Leave it on for 45 minutes and then rinse with warm water and dry thoroughly. Do this twice daily. If you prefer, you can apply this skin cream before bed and let it dry and then leave it on overnight.
Treating Dry Feet
If you are concerned about having dry feet or have any questions about what products are safe to use on your feet, then you should book an appointment with Dr. Vikki and Dr. Connie of the Superior Foot and Ankle Care Center. With years of collective experience in their field, they will be able to help you find the best products to use on your feet.
If you’ve noticed that your toes have been looking a little strange to you lately, or that they have become unusually rigid and tight, you may have hammertoes. A hammertoe is as unpleasant as it sounds: as the namesake suggests, a hammertoe is a deformity which causes the toes to bend sharply downwards rather than straightforward, resembling the silhouette of a hammer.
It is a common but painful condition affecting over 200,000 Americans per year, typically resulting from years of wearing ill-fitting shoes with narrow toe boxes, such as fashionable heels. Fortunately, hammertoe is easily diagnosed and treated, if you know what to look out for. Here is a look at hammertoe causes, symptoms, and treatment:
What Is Hammertoe?
While hammertoe can affect any of the toes, it is most commonly seen afflicting the second, third, or fourth toe. This deformity results when the middle joint of the toe becomes dislocated, forcing the toe to bend sharply downward and buckle in this position. The underlying cause is a muscle and ligament imbalance surrounding the toe joint, where the muscles have tightened from being forced into a flexed position – such as when wearing cramped shoes – to the point where they can no longer straighten out. Pain can result from excessive friction and rubbing against the top of the deformed toe, and corns and calluses may form to further exacerbate the condition.
A number of factors can contribute to the development of hammertoe:
- An uncommonly high foot arch
- Flat feet
- Cramped or ill-fitting shoes
- Pressure from a bunion
- Toe injury
- Arthritis
- Tight tendons or ligaments in the feet
Symptoms & Diagnosis of Hammertoes
Hammertoe is easily recognizable, but you’ll want to confirm with a podiatrist for an official diagnosis. Common symptoms which indicate hammertoe include:
- Pain when walking
- Pain when stretching the affected toe
- A toe which bends downwards and is difficult to move
- Difficulty wiggling the toes or flexing the foot
- Calluses or corns
- Toes taking on a claw-like appearance
There are two types, or stages, of hammertoes: flexible and rigid. A flexible hammertoe means that the condition was caught within its early stages, where the toe is still able to move at the middle joint. This form of hammertoe is still mild, and has a number of various treatment options available. When the condition progresses to the point where the tendons become rigid enough to push the joints out of alignment, the toe will become immovable. At this stage, surgery is usually required.
Your podiatrist can often visually diagnose hammertoe with a physical exam. However, if you’ve had a toe injury, imaging tests may also be required.
Hammertoe Treatment & Prevention
The course of treatment depends upon how far your hammertoe has progressed.
Mild hammertoe that has been caught in its early stages and still remains flexible has a much greater variety of treatment options available. The first step is identifying the cause responsible for the hammertoe. If cramped footwear is the issue, simply switching to better shoes can remedy the condition. If flat feet or high arches are to blame, custom insoles or toe pads can offset the damage. For corns, over-the-counter medications or pads may suffice. Again, consult a podiatrist to determine the source of your hammertoe, to properly advise you on the appropriate treatment option.
Severe hammertoe that has become rigid and inflexible will require surgical intervention to restore motion to the toe. Hammertoe surgery may involve repositioning of the toe, removal of damaged bone, and realignment of the tendons.
The best prevention tip for hammertoes is to make sure that your shoes are fitting properly, and that your feet’s special needs are met. This means getting insoles or orthotics if you require them, and ensuring that your shoes are not too snug nor the heels too high. In general, it is recommended to avoid any heel over 2 inches in height. If you notice any pain, discomfort, or deformity, consult a podiatrist at your earliest convenience to avoid further complications.
Schedule a Consultation with Dr. Vikki and Dr. Connie
If walking has become painful and you suspect that hammertoes are to blame, schedule a consultation with trusted podiatrists Dr. Vikki and Dr. Connie at the Superior Foot & Ankle Care Center today.
Massage therapy has long been lauded as an effective treatment for relieving muscle tension, pain, and stress, but research suggests that the scope of its health benefits go much further. While there are different schools of massage therapy, from Swedish massage to shiatsu, all schools involve applying various levels and techniques of pressure to the muscles in order to promote relaxation. When performed by a trained professional, massage therapy can help resolve muscle damage and even prevent injury.
Foot massage is especially important, as the feet are among the most overused and under-cared for parts of the body. Foot massage techniques are deeply rooted in the study and traditions of reflexology, an alternative medicine discipline that focuses on stimulating pressure points in the feet which correspond to specific systems in the body.
The proven stress reduction stemming from reflexology techniques is then extended to alleviating the symptoms of various ailments and conditions. While a foot massage in itself may not be a cure-all, its stress-relieving and muscle-soothing benefits have far-reaching positive effects on your health, from improved circulation to better sleep.
Here is a look at a few reasons why you should schedule a foot massage regimen:
Stress Relief
The strength of massage therapy as a treatment lies in the healing power of the human touch.Massage reduces the levels of cortisol in the body, the hormone responsible for the negative impact of stress. Moreover, massage has also been shown to improve the levels of serotonin and dopamine which are central to depression. Studies have also found massage to be correlated with increased levels of oxytocin, the hormone intrinsic to emotional bonding.
Thus massage not only relieves the physical tension associated with stress, but the sensation of repeated human touch given in a safe environment produces positive emotions proven to improve symptoms of depression and anxiety. But don’t feel restricted to a professional massage therapist: the emotional benefits associated with massage are just as – if not more – accessible when performed by a loved one.
The benefits of this stress release are expansive: massage can be used as an effective treatment for conditions in which depression and anxiety are the primary symptoms, for example the hormonal changes experienced during PMS and menopause. For this reason, massage has also proven useful in treating migraines and headaches caused by chronic stress. While massage isn’t intended to replace medication for a condition in which depression is a symptom, it is an extremely effective therapy to supplement medical treatment.
Improved Circulation
A 10-20 minute foot massage before bed can work wonders in improving your blood circulation. The kneading pressure applied during a massage helps to improve blood flow through congested areas, allowing fresh blood to flow in. The motions of squeezing and pulling work to clear the muscles of lactic acid, while improving lymph circulation to clear your system of metabolic waste. Better circulation improves blood flow, lowers blood pressure, and enhances overall body function. This is especially helpful for diabetic patients, who struggle with poor circulation in their lower extremities.
Relieves Pain While Reducing Injury
Just 10 minutes of massage following a workout can help reduce inflammation, allowing your body to recover more effectively. Combining strengthening exercises, stretching, and regular foot massages not only facilitates the recovery of existing foot injuries, but helps prevent new injuries from occurring.
Moreover, regular foot massage with deep pressure applied to the arch can alleviate the pain associated with any deformity or weaknesses in the foot, such as with flat feet and plantar fasciitis.
Better Sleep
Due to its expansive stress relieving benefits, foot massage has also been shown to enable relaxation and improve sleep in patients who find it difficult to rest otherwise. This includes individuals who are under chronic stress or struggle with insomnia. Massage therapy has even been shown to improve the rest of patients undergoing chemotherapy. New parents will also be pleased to find that basic massage techniques can even work on newborns, coaxing finicky infants to sleep.
Schedule a Consultation with Dr. Vikki and Dr. Connie
Don’t wait until your foot health is compromised to take advantage of the benefits foot massage has to offer. Schedule a consultation with trusted podiatrists Dr. Vikki and Dr. Connie at the Superior Foot & Ankle Care Center to learn more today.
Despite the way our species evolved away from climbing trees to walking on flat ground, some people are still walking around with monkey-like feet. In fact, you may be surprised to learn that about eight percent of the population, or 1 in 13 humans, may have a midtarsal break in their foot characteristic of non-human primates. These are also referred to as prehensile feet.
What is a Midtarsal Break?
The midtarsal break is a medial shift in the center of the pressure trajectory with dorsiflexion of the midtarsal joint (the joint between the talus and the navicular bone as well as the joint between the calcaneus and the cuboid bone), occurring during the gait of an unstable foot, when the body transfers weight from rearfoot to forefoot.
A midtarsal break, also known as floppy feet, tend to occur in people with flatter feet and higher body mass indexes than people with stiffer feet. They also tend to roll their feet more, causing a motion called hyperpronation (they land on the outside of their feet and roll dramatically inward). This allows for the foot to relax its joints and ligaments, creating a midtarsal break.
What are Prehensile Feet?
Prehensile feet are lower limbs that possess prehensility (the ability to grasp like a hand). They are most commonly observed in monkeys. Due to the development of bipedalism in humans, the hands became the focus of prehensility and the feet adjusted to more of a stabilizing role. It may be possible, however, that the foot does not reach its limits of dexterity due to the constant muscle tension needed in stabilizing and balancing the foot to hold up the legs and the rest of the frame.
People with prehensile feet can grasp small objects between their toes, manipulating them as with a hand with the ankle functioning like the wrist. As toes are much shorter than fingers, and since the ball of the foot is so large and obtrusive, grasping does not function as in a normal hand and the foot is not able to hold very large or heavy objects.
Chimpanzee Feet vs. Human Feet
Conventional wisdom has always claimed that the human mid-foot is rigid, which allows for more efficient walking while chimpanzees and other apes have flexible feet better suited to grasping branches as they move through the trees.
Human feet are both rigid and pliable depending on the need. The human foot is a spring arch that should be able to drop and lift with every step. Human legs angle in from the hip to the knee, allowing our feet to fall directly under the pelvis and our pelvic muscles are much stronger, as well, allowing for a stable upright environment.
Chimpanzees are often referred to as knuckle-walkers because they only walk on two legs for short distances due to the differences of our legs and spine. Chimpanzees can’t straighten their legs like humans and they don’t have a lumbar curve, which makes weight bearing and walking more difficult. Chimpanzee legs are also set wide apart and weak pelvic muscles force their whole body to transfer weight from side to side during each step.
Yet, while chimp feet and bodies can’t do what humans can, it doesn’t appear to be a problem if our feet work like chimpanzee feet. In fact, two studies (one from Boston University and the other from Dartmouth) have proven that about eight percent of the population have the mobility of chimpanzee feet, which allows some societies to functionally adapt their feet and calf muscles to allow them to climb trees like chimps do.
While eight percent of the population exhibits a flexible midtarsal break in their feet, people with midtarsal break rarely realize that they have one, as it doesn’t affect their gait.
The Walking Test
So how do you know if your feet might have a midtarsal break? Take a stroll on sand. Here are a couple of tips:
- If you have high arches, you probably have stiff muscles and ligaments, which means that you don’t have a midtarsal break.
- If you have a midtarsal break, the fold in your foot will pinch the sand upward. Look for a small ridge in the upper-mid portion of your footprint.
Talk to Dr. Vikki and Dr. Connie
If you have any questions or concerns about whether or not you have prehensile feet with a midtarsal break, and if there are any unique factors you have to account for regarding your foot health, feel free to book an appointment with Dr. Vikki and Dr. Connie today.
Skin on the feet or ankles can discolor for any number of reasons, ranging from staining from wet clothes or boots to serious medical conditions. Yet, if the discoloration isn’t immediately explainable by simple environmental factors, then it’s in your best interest to seek medical attention.
Here are some things that you should know about some of the more serious problems that could be causing your feet discoloration.
Venous Insufficiency
Venous insufficiency, also known as chronic venous insufficiency or chronic venous stasis, is a problem with the flow of blood from the veins of the legs back to the heart. This occurs when the valves in the veins of the leg don’t work properly, causing fluid pools to form, which can lead to other problems including varicose veins.
Venous insufficiency can be caused by blood clots, deep vein thrombosis, or high blood pressure inside the leg veins. You are more likely to have venous insufficiency if you:
- Are older
- Are female
- Are overweight
- Don’t get enough exercise and tend to lead a sedentary lifestyle
- Smoke
- Have a family history of varicose veins
Symptoms may include:
- Swelling, often in the ankles
- Varicose veins
- Itching
- Cramping
- General weakness
- Skin sores (ulcers)
- Aching or a feeling of heaviness
- Changes in skin color/feet discoloration
- Thickening of the skin on your legs or ankles
In order to treat venous insufficiency, your doctor may ask you to:
- Wear compression stockings
- Get more exercise (especially walking)
- Avoid standing or sitting for long periods of time
- Keep your legs elevated when lying down
In more severe cases, you may have to undergo surgery to correct venous insufficiency. Your doctor may suggest one of the following types of surgery:
- Surgical repair of veins or valves
- Removing (stripping) the damaged vein
- Minimally invasive endoscopic surgery—the surgeon inserts a thin tube with a camera on it to help see and tie off varicose veins
- Vein bypass—a healthy vein is transplanted from somewhere else in your body (this procedure is generally used when the upper thigh is affected and only for very severe cases after nothing else has worked)
- Laser surgery—uses lasers to either fade or close the damaged vein(s) with strong surges of light in a small, specific place. It involves no surgical cuts.
Rocky Mountain Spotted Fever
Rocky Mountain spotted fever is a bacterial infection transmitted by a tick. Without prompt treatment, Rocky Mountain spotted fever can cause serious damage to internal organs, such as your kidneys and heart.
Although many people become ill within the first week after infection, signs and symptoms may not appear for up to 14 days. Symptoms can include:
- High fever
- Chills
- Severe headache
- Muscle aches
- Nausea and vomiting
- Restlessness and insomnia
- Rash—the red, non-itchy rash typically appears a few days after the initial signs and symptoms begin. It first appears on your wrists and ankles, and can spread in both directions.
People who develop Rocky Mountain spotted fever are much more likely to avoid complications if treated within five days of developing symptoms.
Ankle Sprain
An ankle sprain is an injury to the tough bands of tissue (ligaments) that surround and connect the bones of the leg to the foot. The injury typically occurs when you accidentally twist or turn your ankle in an awkward way. This can stretch or tear the ligaments that hold your ankle bones and joints together.
Symptoms of an ankle sprain can include:
- Swelling
- Bruising
- Pain
- Inability to put weight on the affected ankle
- Skin discoloration – primarily ankle and foot discoloration
- Stiffness
Treating a sprained ankle is important to promote recovery and to prevent further discomfort. If your sprain is mild, you should be able to treat it at home by:
- Using elastic bandages to wrap your ankle
- Wearing a brace to support your ankle
- Using crutches
- Elevating your foot with pillows while resting or sleeping to help reduce swelling
- Taking ibuprofen (Advil) or acetaminophen (Tylenol) to manage swelling and pain
- Getting plenty of rest and not putting weight on your ankle
- Applying ice every 20-30 minutes, three to four times per day
Surgery for ankle sprains is rare, but it may be performed when the damage to the ligaments is severe or when the injury doesn’t improve with non-surgical treatment. Surgical options include:
- Arthroscopy—your doctor will look inside the joint to see if there are any loose fragments of bone or cartilage
- Reconstruction—you doctor will repair the torn ligament with stitches. They may also use other ligaments or tendons around the foot or ankle to repair the damaged ligaments.
Proper Diagnosis
If you’re experiencing any feet discoloration, and the cause is not immediately known to you, you should seek out medical attention. A proper diagnosis can go a long way to helping you treat and quickly recover from whatever is causing your foot discoloration.
If you have any questions or concerns about feet discoloration, book an appointment with Dr. Vikki and Dr. Connie, so that they can help you get the right answers and treatment.
Whether you’re trying to help out a friend or you’ve hurt your own foot, knowing how to properly deal with and take care of an injured foot can save you a lot of stress and problems later.
Here’s a quick how-to guide on how to properly take care of and bandage an injured foot or ankle.
How to Stop Any Bleeding
If there is any blood involved, it is important to first wash your hands and put on medical gloves (if available) before applying direct pressure to the wound. If gloves aren’t available, use many layers of clean cloth, plastic bags, or the cleanest fabric available between your hands and the wound.
In order to stop the bleeding, you should:
- Have the injured person lie down and elevate their foot for a full 15 minutes
- Remove any visible objects in the wound that are easy to remove
- Remove clothing and jewelry from the general area of the wound in case of swelling
- If blood soaks through the cloth, apply a clean one
How to Wrap an Injured Foot or Ankle
To prevent further injury and encourage proper healing, you should make sure that you protect and compress your foot, as well as rest, ice, and elevate your injury. There are a couple different types of material that you can use to wrap and compress an injured foot or ankle, including an elastic cloth bandage and athletic tape.
Wrapping with an Elastic Cloth Bandage
- Begin wrapping—place the end of the bandage where the toes meet the foot. Begin by wrapping the bandage around the ball of the foot. Hold the end of the bandage against the ball of the foot with one hand, and use the other to bring the tail around the foot from the outside. Make sure to keep the bandage tight, but not so tight that it decreases blood flow to the foot and toes.
- Work your way toward the ankle—wrap the ball of the foot twice, to hold the bandage in place, then begin moving up towards the ankle, being sure to leave at least one-half inch of bandage overlapping the previous layer. Make sure the layers are smooth and even with no unnecessary bulges or lumps. Start over if you need to do the job more neatly.
- Wrap the ankle—when you get to the ankle, bring the end of the bandage up outside of the foot, over the instep and around the inside of the ankle. Then bring it around the heel, back up over the instep, under the foot and around the ankle. Continue making a figure eight around the ankle several times to fully stabilize the ankle.
- Finish the wrap—the last wrap should rise several inches above the ankle to help stabilize it. Use the metal fasteners or medical tape to secure the remaining bandage. Excess bandage can also be tucked under the last layer, provided there’s not too much excess.
Wrapping with Athletic Tape
- Decide if athletic tape is right for you—while athletic tape works to wrap an injured ankle, it is primarily made to wrap an uninjured joint before physical activities to avoid injury, not to protect an already injured ankle.
- Begin with an underwrap—underwrap is a non-adhesive material used to wrap the foot and ankle before tape is applied, so that the tape doesn’t pull at the surface of the skin. Starting at the ball of the foot, wind the underwrap around the foot up to the ankle, leaving the heel uncovered.
- Secure the anchor—cut the strip of tape long enough to wrap one and a half times around your ankle. Wind it around your ankle, over the underwrap, to hold the underwrap in place.
- Create a stirrup—place the end of a piece of tape on one side of the anchor. Bring it down under the arch of the foot and back up to the other side of the anchor. Press it lightly to secure it in place. Repeat with two more pieces of tape overlapping the first one to create a sturdy stirrup.
- Create an X over the foot—place the end of a piece of tape at the ankle bone and run it diagonally over the top of the foot. Bring it down under the arch and toward the inside of the heel. Then bring it around the back of the heel and back up over the foot to create the other part of the X.
- Make a figure eight—place the end of a piece of tape on the outside of the ankle, just above the bone. Run it over the top of the foot at an angle, then bring it under the arch and up the other side of the foot. Next bring it around the ankle and back to the point where you started. Use another piece of tape to make a second figure eight that overlaps the first one. This will ensure that the wrap is held securely in place an provides enough support for the ankle to heal properly.
If a foot or ankle injury is serious and/or life-threatening, it’s important to call an ambulance. However, if the pain is manageable and you need help in dealing with the injury and getting back on your feet as soon as possible, be sure to get in contact with Dr. Vikki and Dr. Connie today.
More...
There are some professions out there that cause a lot of stress to the arches, balls and heels of the feet, which can lead to other spinal and back discomfort issues, fatigue, and various mental health problems. Health care professionals, construction, hairdressing, office jobs, as well as landscaping jobs are all very different professions with this commonality—all are very stressful for the feet and can cause foot problems and pain.
Health Care Professionals
Hospitals are one of the busiest public places where employees work long hours. Nurses and doctors are always on the move during their long shifts, walking miles each day to serve and assist their patients. This can lead to numerous foot problems such as bunions, flat feet, ingrown nails, and heel spurs.
The foot has dozens of bones, joints, muscles, nerves, blood vessels, tendons, and layers of connective tissue. When working in the health care profession and working those long hours on your feet, the body tissues in your feet can become very stressed, achy, and swollen. If there is prolonged inflammation, this will actually form scar tissue and tire out the bones of the feet.
For those that work in the healthcare profession, be sure to wear comfortable, arch-supportive shoes with shock-absorbing soles, and get them fitted by a professional to make sure they are exactly right for your feet.
Construction Workers
Construction work is a heavy-duty, active profession that puts a lot of strain on the entire body, including the feet. Construction workers have to work in very challenging weather and circumstances and are on their feet for their entire day besides some small breaks. They are required to bend and lift and tend to end their shifts very exhausted and, sometimes, in pain.
The most common injury experienced by construction workers are ankle and foot injuries. Construction workers often develop flat feet or severely painful arch problems that can hinder their performance and their lifestyle outside of work.
Construction workers should invest in good footwear, such as steel-toe boots, that are a high quality brand able to prevent blisters, calluses, and protect the feet from anything heavy that could fall on them. Weeks before working in new boots, it’s key to break them in as much as possible.
If construction workers experience a foot injury, they should take days off to recover and see a medical professional like a podiatrist who can identify the problem and prevent further pain and injury.
A great tip is to freeze a bottle of water before heading out to work. When you get home, roll your feet over the frozen bottle. Not only will this exercise reduce inflammation and pain, but also the motion of the rolling will get the blood moving in your feet.
Hairdressing
Hairdressers often complain of foot pain at work, and this can result from repetitive straining motions; but also from a lack of supporting your feet and preventing foot problems well before pain and problems occur. If you are a hairdresser, try to remember to not lean on one dominant side when cutting hair.
Try to ground yourself and distribute your weight evenly on both of your feet. This will prevent pinched nerves and developing uneven arches.
Another way to prevent foot problems is to exercise and have a balanced diet. The more weight you carry, the more strain that’s placed on your feet, legs, and back. It’s simple—the more you weigh, the harder it is for you to be standing on your feet day all day.
Invest in a rubber mat for your chair and work space area. This will prevent developing foot problems and will keep your back healthy, too. Wear good shoes with less than a 1.5-inch heel to avoid severe heel pain. Absorbent pads and laces on the body of the shoe can help provide optimal support. Consider orthotics if you’re already experiencing foot pain as this will alleviate and correct current problems.
Preventing Foot Problems
Healthy feet are the key to a healthy life. Talk to a podiatrist professional such as the great team at the Superior Foot and Ankle Care Center and learn more about what you can do to keep your feet healthy.
Foot Inflammation is the body’s attempt to fend off foreign, invasive objects, including bacteria or viruses. In other words, inflammation is an immunological response to remove potentially harmful foreign stimuli and to heal the site of invasion.
Inflammation often begins with irritation, and is then followed by suppuration (pus discharge). Then there is the granulation stage – the formation in wounds of tiny, rounded masses of tissue during healing.
Symptoms of inflammation include redness, swelling, pain, localized stiffness, and loss of functions. These symptoms may not often be concurrently present. Inflammation may also cause flu-like symptoms including fever, chills, fatigue or lethargy, headache, loss of appetite, and muscle stiffness.
Common Causes of Foot Inflammation
Foot inflammation is caused by injury, overuse, or other conditions causing inflammation of the bones, ligaments, or tendons in the foot. A list of common causes for foot pain can include, but are not limited to, the following:
- Achilles tendinitis
- Arthritis
- Bone spurs
- Broken ankle/broken foot
- Bunions
- Corns and calluses
- Diabetic neuropathy
- Gout
- Hammertoe and mallet toe
- High heels or poor-fitting shoes
- Ingrown toenails
- Osteoarthritis
- Paget’s disease of bone
- Peripheral neuropathy
- Plantar fasciitis
- Plantar warts
- Stress fractures
Preventing Foot Inflammation
As necessary and inevitable as it is that we rely on our feet for mobility to engage in daily activities, there are many ways in which we can care for our feet so they continue to support us without causing us pain:
- Maintain a healthy weight: As the weight-bearer of the body, the more weight our feet have to support, the more stress they are put under. As little as 20 extra pounds on your body will change the way your feet function, increase the stress on your feet, and possibly trigger pain. If foot pain occurs during exercise, try switching to a low-impact sport such as swimming.
- Boost flexibility: Stretch the calf muscles on a regular basis, as they tend to tighten as you age, thus putting extra stress on your feet. Try the following calf-stretching exercise three times a day:
- Stand with your toes on a step with your heels of the edge.
- Slowly lower your heels and hold for 10 seconds; lift your heels to the starting position.
- Repeat five to 10 times.
- Do not force your heel farther than what feels comfortable. Complete the exercise one foot at a time if necessary.
- Avoiding high-heels: Wearing high-heels shortens calf-muscles and increases the likelihood of experiencing back pain. One study found that it takes only 66 minutes of wearing heels for the pain to kick in. Moreover, forcing your feet into pointy-toed heels can cause foot ailments such as ingrown toenails, bunions, blisters, and deformed toes.
- Ensure a comfortable fit: Feet change in shape in size as you age, so it is important to have your feet measured before you purchase a new pair of shoes. In addition, it is common to have feet of different size; therefore, be sure to have both feet measured and buy the size that fits the larger foot. Before purchase, also make sure there is about half an inch of wriggle room between your longest toe and the front of the shoe. Shop for shoes in the afternoon when your feet are usually at their largest, and wear the socks you would normally wear with the particular type of shoes.
- Take seated breaks: If you need to be on your feet most of the day, try to take seated breaks during which your feet can rejuvenate.
- Trim your toenails with care: Ingrown toenails are a common source of foot pain. Cut your toenails straight across; do not cut around the corners to match the shape of your toe.
- Stay hydrated: Dehydration can cause foot cramps, which can come on suddenly and cause sharp, debilitating pains. Drinking plenty of fluids, and eating food rich in potassium such as bananas and spinach will minimize the risk of experiencing foot cramps.
If you’ve taken the above steps and find that your foot inflammation is not alleviating itself, be sure to get in contact with Dr. Vikki and Dr. Connie today.
Do you find that you often have back or joint pain? Has anyone ever told you that you have terrible posture? The two are connected, and both have a lot to do with your feet.
Improper foot alignment can cause an array of problems, but you don’t have to live with them forever. Here are some quick tips on how to fix your posture by focusing on your feet.
How the Feet Work
Before you can learn how to fix your posture by focusing on your feet, it is important that you understand the feet themselves. Each foot has 26 bones, 33 joints, and more than 100 muscles, tendons, and ligaments. The foot is divided into three parts: the hind foot (the ankle bone and the heel bone), the mid foot (a group of five irregular bones in the arch of the foot), and the forefoot (the metatarsals and toes).
Our feet move in different ways:
- Plantar flexion of the ankle, which occurs when you stand on tiptoes. If you’re sitting with your legs out in front of you, plantar flexion of the ankle happens when you point your toes.
- Dorsiflexion, which occurs when you stand on your heels with the balls of your feet lifted off the floor. If you’re sitting, dorsiflexion happens when you push your heels away from you and pull your toes toward you.
- Supination, which takes place when you stand with your weight rolled onto the outer edges of your feet, lifting the arches and the base of the big toe. Non-weight bearing supination happens when you sit with your legs out in front of you and turn the soles of the feet so they start to face each other.
- Pronation, which happens when you lift the outer edges of your feet as you stand, collapsing your arches. In sitting postures, pronation occurs when you press out through your inner heels and the bases of your big toes.
Correct distribution of weight in your feet can help give your body optimal postural alignment.
Common Problems and How to Fix Them
Two of the most common foot problems that can affect your posture are pigeon toes and duck feet.
Pigeon Toes
Cause: Weak glutes (butt muscles) and overactive tensor fasciae latae (outside of your hip).
Fix: Lie on one side with your knees bent 90 degrees and your heels together. Keeping your hips still, raise your top knee upward, separating your knees like a clamshell. Pause for five seconds, then lower your knee to the starting position. That’s one rep. Perform two or three sets of 12 reps on each side daily.
Duck Feet
Cause: Weak oblique muscles and hip flexors, and overactive piriformis and the other deep external rotators (muscles really deep in your hip attaching the femur to your sacrum).
Fix: Get into a push-up position with your feet resting on a stability ball. Without rounding your lower back, tuck your knees under your torso, using your feet to roll the ball toward your body, then back to the starting position. That’s one rep. Do two or three sets of six to 12 reps daily.
Making Small Changes
While exercising your feet can definitely help with your overall posture, you should also consider making small changes to your everyday life. Some of the things that you can do include:
- Being aware—take a while to study how you stand, or have your doctor on your next visit look at your legs and their alignment. A yoga therapist, chiropractor, or podiatrist with an extensive background in anatomy and physiology can do this for you, as well.
- Make adjustments—your body might just need a change in how you walk. For example, if you notice you walk more toward your instep, adjust how you walk on your own. Find that correct distribution of weight and movement in your feet.
- Build muscle strength and relaxation—if you have fallen arches, those muscles might be weak, work on them with yoga poses specifically targeting those muscles in the lower legs. In turn, some muscles may be too strong, pulling your leg and pelvis in a certain direction. Work on relaxing those in addition to building strength in your weaker sections.
- Use traction exercises—traction, when done manually with a strap or belt, can be a great way to gently work your problem areas back to their most favorable shape, strength, or position.
- Walk barefoot—our feet were made to walk just as they are. Putting them in heels or tennis shoes brings the foot into an unnatural shape, no matter how much they are advertised to be good for walking, running, or any other activity.
- Try not to rely on insoles—you can have customized insoles for your shoes, and although they do make you feel better when you wear your shoes, they can’t always completely fix the problems that you’re having.
- Be kind—treat your feet with kindness. Remember to massage your feet to release tension. Using a hard rubber ball under the soles and moving the foot back and forth works wonders.
Treating Improper Posture with Dr. Vikki
Since fixing the way your feet take your weight can help correct your overall posture, it is important that you have your feet properly examined by an experienced podiatrist. Book an appointment with Dr. Vikki and Dr. Connie today, so that they can help you get your feet back on the right track.
A foot fracture occurs when one or more of the 26 bones of the foot break as a result of either a sudden trauma or chronic overuse. In general, foot fractures come in two broad categories:
- Full foot fracture: typically a result of a one-time trauma to the foot, such as a car crash or impact from a blunt and heavy object to the foot.
- Stress fracture: caused by repeated stress to a bone or multiple bones in the foot, a stress fracture may sound less severe than a full foot fracture, but it still entails a breakage of the bone in the foot.
There are, in addition, different types of bone fractures depending on their nature:
- Non-displaced: when a bone breaks but stays in place.
- Displaced: when a bone breaks into two pieces that move apart from one another.
- Comminuted: when a bone is broken in multiple places in the foot.
- Open fracture: when a bone breaks through the skin after fracturing.
Home Treatment for a Foot Fracture
If you suspect that a fracture might have occurred, it is best to err on the side of caution and apply first aid treatment to the affected foot. The acronym RICE can help you remember what to do in such a situation:
Rest: Rest the affected area. Stay off the injured foot until it can be fully evaluated. Walking, running, or playing sports on an injured foot may exacerbate the injury.
Ice: Apply ice to the affected area as soon as possible, and reapply it for 15–20 minutes every three or four hours for the first 48 hours after injury. Ice helps decrease inflammation.
Compression: Wrap an elastic bandage around the affected foot. The wrapping should be snug, but not so tight as to cut off circulation.
Elevation: Elevate the affected extremity; ideally, your foot should be elevated higher than your chest/heart area. Keeping your foot elevated decreases blood flow to the area, and thus decreases swelling.
Using nonsteroidal anti-inflammatory drugs such as ibuprofen or naproxen can help relieve pain and reduce swelling.
Visiting a Podiatrist for a Foot Fracture
If you notice increased pain, swelling, bruising, redness, or difficulty walking after an injury, you should see a podiatrist immediately. A podiatrist will take a complete medical history while examining your foot to look for areas of tenderness by applying gentle pressure directly to the injured bone. Often, the key to diagnosing a stress fracture is the patient’s report of pain in response to this pressure.
The podiatrist may then order tests, including an X-ray, ultrasound, or MRI, to determine the extent of your injury. You may not need further testing beyond an X-ray if it clearly indicates the location of the fracture. Otherwise, ultrasounds and MRIs will be useful for finding soft issue injuries (including torn ligaments) and fractures that might not have shown in an X-ray.
Treatment Options for Foot Fractures
Treatment for a foot fracture will depend on your injury. If you have a broken bone, your podiatrist may attempt to reduce the fracture by lining up the ends of the bones so they can heal properly (reduction). You’ll be given a local anesthetic to numb the area should this be your treatment option.
An unstable fracture in which the ends of the bone do not stay in place after a reduction may require surgery. Internal fixation is the procedure during which pins, screws, and/or metal plates are used to hold the small bones of the foot together during the healing process.
Caring for a Fractured Foot
Your podiatrist may recommend that you use crutches to keep weight off your foot until the pain subsides. Other recommendations for caring for your injury during the healing process include:
Modified activities. It typically takes from 6 to 8 weeks for a stress fracture to heal. During that time, switch to activities that place less stress on your foot and leg. Swimming and cycling are good alternative activities; although you should not resume any type of physical activity that involves your injured foot or ankle – even if it is low impact – without your podiatrist’s recommendation.
Protective footwear. To reduce stress on your foot and leg, your podiatrist may recommend wearing protective footwear. This may be a stiff-soled shoe, a wooden-soled sandal, or a removable short-leg fracture brace shoe.
Casting. Stress fractures in some of the bones of the foot, such as the fifth metatarsal bone (on the outer side of the foot), take longer to heal. Your podiatrist may apply a cast to your foot to keep your bones in a fixed position and to remove the stress on your involved leg.
If you believe you’ve suffered a fracture anywhere in either of your feet, be sure to get in contact with Dr. Vikki and Dr. Connie at the Superior Foot and Ankle Care Center.